Each year, an estimated 20,000 to 25,000 individuals with penises in the United States receive penile implants to treat erectile dysfunction.
Despite high demand, mastering penile prosthesis surgery remains challenging due to limited access to cadaver models for training.
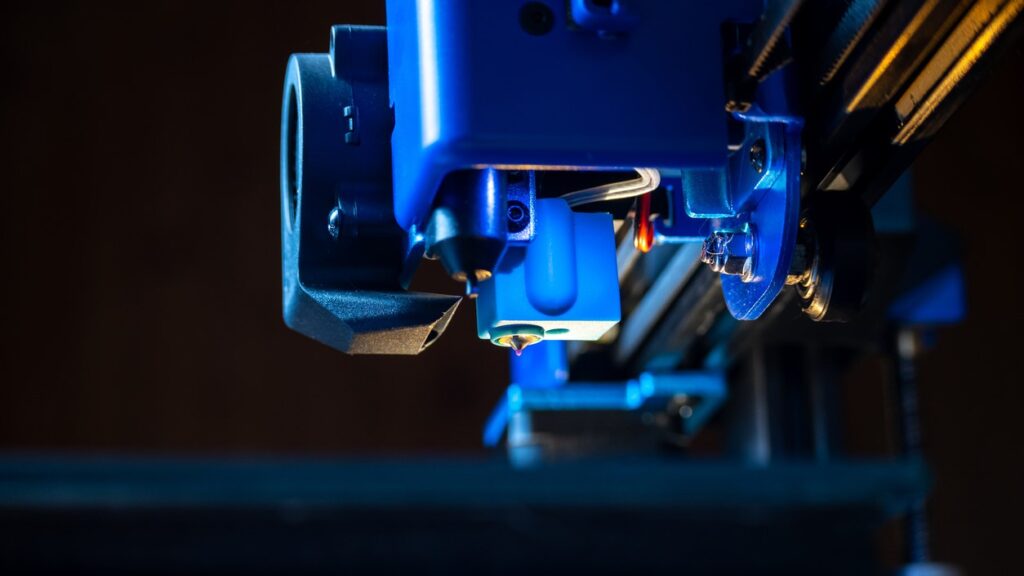
Enter 3D-printed models, a cutting-edge solution that allows surgeons to hone their skills before stepping into the operating room. A study published in The Journal of Sexual Medicine uncovers their potential as a low-cost and ethical option to enhance penile prosthesis surgery training.
Cadavers vs 3D models
Dissecting cadavers is considered the “gold standard” for learning anatomy, but there are drawbacks. They are expensive to use, limited in supply, and require safe disposal.
In this study, experienced penile surgeons from the European Society for Sexual Medicine tested a 3D model for training against cadaver models.
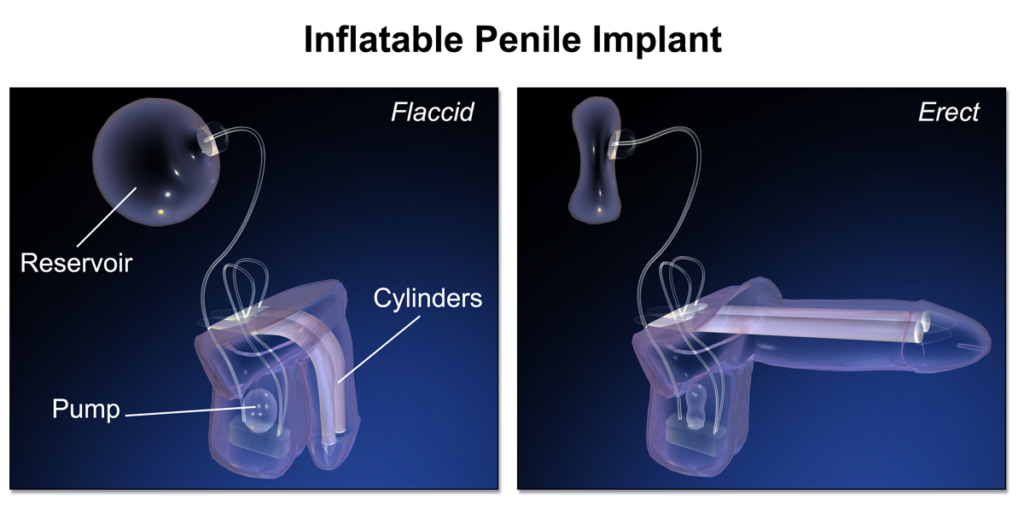
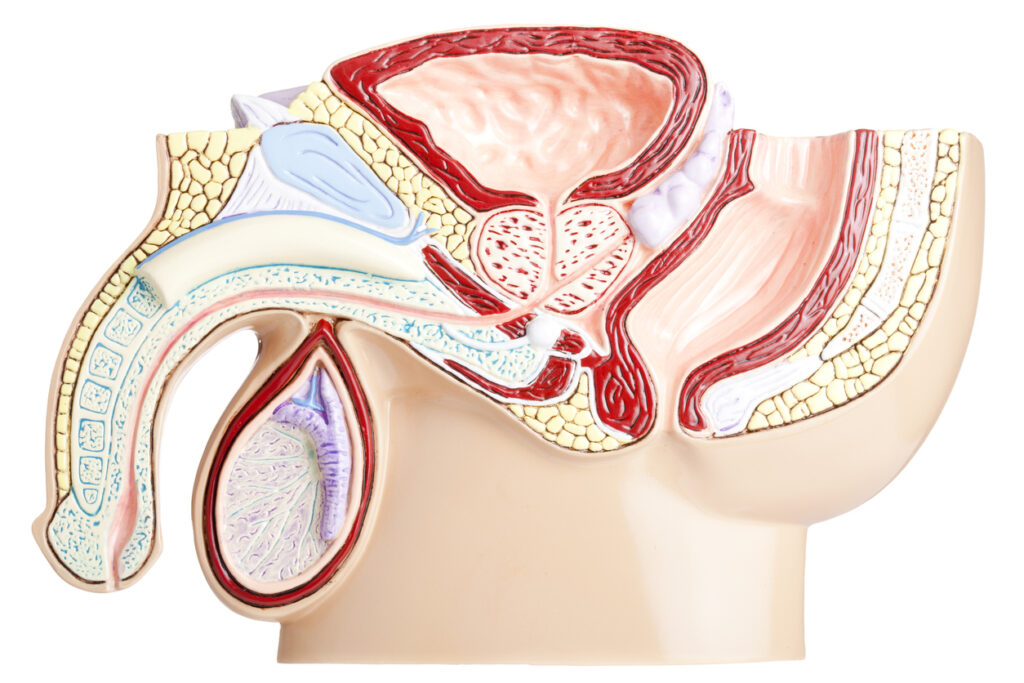
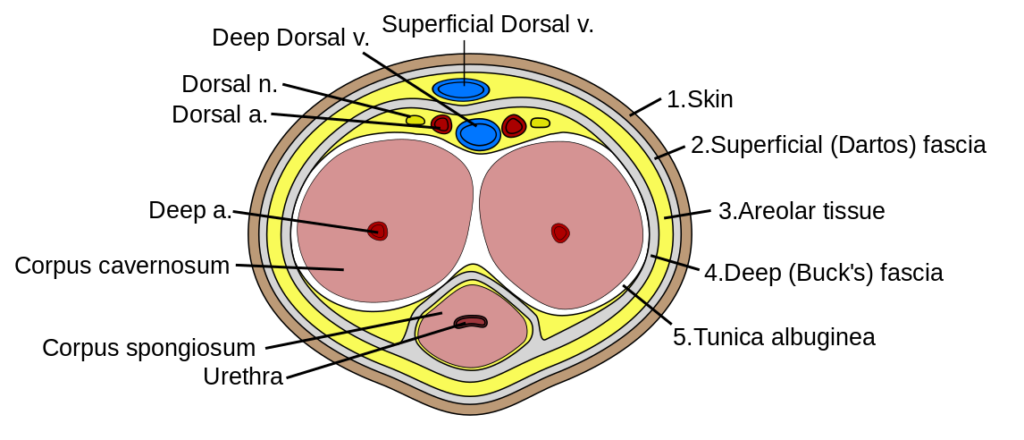
The University of Rochester’s Simulation Innovation Lab developed the male pelvic model using hydrogel, polymer molding, and 3D printing. Based on MRI data, it replicates key anatomical structures such as the urethra, scrotum, and major blood vessels.
The study involved three stages.
First, two experts checked the 3D model’s accuracy against a cadaveric pelvis. Following their feedback, the Simulation Innovation Lab refined the model by resizing the inguinal canal and adding colored fluid to the blood vessels.
Second, three experts evaluated the improved 3D model’s anatomical accuracy and teaching suitability using the Rochester Evaluation Score. This tool is used to assess medical training models, particularly surgical and procedural simulations.
Third, three experts evaluated the improved 3D model’s effectiveness for surgical training and skill acquisition. They simulated penile implant surgeries and assessed them using a modified questionnaire from ear-nose-throat surgery and the Rochester Evaluation Score.
Validating the 3D model
The 3D model showed impressive anatomical accuracy and potential for penile prosthesis surgery training. However, the experts flagged a few areas that need improvement.
Second-stage results: Anatomical accuracy
Compared to the cadaveric model, the 3D model earned an average rating of 4.33 out of 5 for anatomical accuracy. Although a high score, two experts said the hydrogel model requires enhanced visibility of Buck’s fascia.
Buck’s fascia is a layer of connective tissue that surrounds the deep structures of the penis. It provides support and helps maintain the shape and function of the penis.
Third-stage results: Surgical skills and training
Experts rated the 3D hydrogel model as highly effective for surgical training.
They gave it an average score of 4.33 out of 5 for improving technical skills, teaching and practicing the procedure, and assessing a surgeon’s ability.
For improving skills and teaching, one expert found the 3D model superior to the cadaver model, while the other two rated them equally. Similarly, for training preference, one expert preferred the 3D model, while the other two rated both models the same.
The experts also recommended adjustments. They included altering the height of the pelvic bone, the elasticity of the inguinal canal, and the structure of Buck’s fascia.
Overall, experts found the 3D model more ethical, cost-effective, and accessible than cadavers.
Practice makes perfect
The 3D hydrogel model holds incredible promise as a tool for learning penile prosthesis surgery.
While experts suggested improvements, the study confirmed its high anatomical accuracy and effectiveness as a training simulator.
By using the 3D model before progressing to cadavers, it could significantly reduce training costs. Allowing more opportunities to practice penile implant surgery will likely lead to increased patient safety and fewer complications.
“The possibility of having an ethical, easy-to-use model with lower costs and limited consequences for the environment is invigorating,” wrote the authors.
“The next step will be validation of the 3D model for penile prosthesis surgery during clinical surgical training and the development of future models to be used in teaching corrective surgery in Peyronie’s disease.”
Beyond penile prostheses, this novel approach stands to reshape surgical education, making it more accessible, affordable, and eco-friendly.
Featured Image Source: iStock